Introduction to nail infections caused by fungal pathogens
Nail infections caused by fungal pathogens are a common condition that affects millions of people worldwide. Fungal nail infections, also known as onychomycosis, occur when fungal organisms invade and colonize the nails. This condition can cause various symptoms, such as discoloration, thickening, brittleness, and distortion of the nails.
Fungal pathogens that cause nail infections typically belong to a group of fungi called dermatophytes. These organisms thrive in warm and humid environments, making nails an ideal breeding ground. Nail infections can also be caused by non-dermatophyte fungi, such as yeasts and molds.
Fungal pathogens penetrate the nails by entering through small cracks or cuts in the skin around the nails or through the tiny spaces between the nail plate and the nail bed. Once inside, they begin to multiply and spread, leading to the characteristic symptoms of nail infections. Fungal nail infections are often difficult to treat and eradicate completely, as the fungi can persist in the nail bed and reoccur if not adequately managed.
Preventing fungal nail infections can be challenging, especially in communal areas like swimming pools, locker rooms, or nail salons where the fungi can be easily transmitted. Good foot hygiene, avoiding prolonged moisture exposure, wearing breathable shoes and socks, and regularly inspecting and trimming nails can reduce the risk of fungal nail infections.
Understanding the anatomy of nails and how they can be susceptible to fungal infections
Understanding the anatomy of nails is crucial when it comes to comprehending how they can be susceptible to fungal infections. Nails, composed of a protein called keratin, protect the sensitive fingertips and toes, but they are also susceptible to a variety of pathogens, including fungus. Fungal nail infections, also known as onychomycosis, occur when fungi penetrate the nail and surrounding tissues, leading to discoloration, thickening, and brittleness.
Fungal pathogens cause nail infections by exploiting conditions that favor their growth. Warm and moist environments, such as sweaty shoes or public swimming pools, create an ideal breeding ground for fungi. The infection typically begins at the free edge or the outer corner of the nail, where the fungi first penetrate and establish themselves. Over time, if left untreated, the infection can spread deeper into the nail plate and may even affect the nail matrix, where new nail cells are formed.
Factors that increase the susceptibility to fungal nail infections include advanced age, weakened immune system, circulation problems, and frequent exposure to damp or humid environments. Additionally, nail trauma, such as repetitive microtrauma from ill-fitting shoes or manicures, can provide entry points for fungal pathogens. It is essential to understand these vulnerabilities to prevent and effectively treat fungal nail infections.
Common types of fungal pathogens responsible for nail infections
Fungal pathogens are the main cause of nail infections, also known as onychomycosis. There are several common types of fungal pathogens that can infect nails, each with their own characteristics and effects.
One of the most common types is dermatophytes, which are fungi that thrive in warm and moist environments. These fungi can invade the nail bed, causing the nails to become thickened, discolored, and brittle. Dermatophyte infections are often accompanied by itching and discomfort.
Another prevalent type of fungal pathogen is Candida, a yeast-like fungus that can infect the nails. Candida infections typically occur in the nail folds or under the nail plate, causing the nails to become thick, brittle, and crumbly. Candida nail infections are more common in individuals with weakened immune systems or those who frequently expose their hands to water or moisture.
Non-dermatophytic molds, such as Scopulariopsis and Aspergillus, can also cause nail infections. These molds are often found in soil and decaying vegetation and can enter the nails through small cuts or abrasions. Non-dermatophytic mold infections may cause the nails to become thickened, discolored, and distorted, and they can be challenging to treat.
It is important to note that identifying the specific fungal pathogen responsible for a nail infection requires a laboratory culture or microscopic examination. Proper diagnosis is crucial for determining the most effective treatment approach, as different types of fungal pathogens may respond differently to specific antifungal medications.
The process of fungal infection: how does it start and spread?
Fungal nail infections, also known as onychomycosis, are caused by different types of fungi, including dermatophytes, yeasts, and molds. The process of fungal infection generally begins when the fungus gains access to the nail bed, which is the area beneath the nail plate. There are a few common ways in which this can occur.
One common route of infection is through direct contact with an infected individual or contaminated surfaces such as shower floors, locker rooms, or nail salons. Fungi thrive in warm, moist environments, making these places ideal for their growth and transmission. Once the fungus enters the area beneath the nail plate, it begins to multiply and spread, leading to an infection.
Another way fungal nail infections can start is by the invasion of the nail bed through a small injury or break in the skin around the nail. This can include minor cuts, nail trauma, or even a separation of the nail from the nail bed. Fungi can easily penetrate these openings and establish an infection, feeding on the keratin in the nails and causing them to become discolored, brittle, and thickened.
As the fungal infection progresses, it gradually spreads to neighboring nails or other areas of the body. Fungi produce spores that can be easily carried by air or touch, facilitating their transmission. Moreover, the warm and damp environment of shoes or socks can further promote the growth and spread of the infection. Without proper treatment, fungal nail infections can become chronic and difficult to eradicate.
Preventing the spread of fungal nail infections involves maintaining good foot hygiene, wearing proper footwear in public areas, avoiding sharing personal items like socks or nail clippers, and treating any minor injuries around the nails promptly. If an infection develops, seeking medical attention for appropriate antifungal treatment is crucial to ensure effective eradication and prevent further spread.
Risk factors and causes: why are some individuals more prone to nail infections?
Nail infections, also known as onychomycosis, are caused by fungal pathogens that invade the nails and surrounding tissues. While anyone can develop a nail infection, certain individuals may be more prone to them due to various risk factors and causes.
One of the primary risk factors for nail infections is weakened immune system. People with conditions such as diabetes, HIV/AIDS, or immunodeficiency disorders are more susceptible to fungal infections, including those affecting the nails. Additionally, individuals who have undergone organ transplants or are taking immunosuppressant medications are at a higher risk.
Poor hygiene practices can also increase the likelihood of nail infections. Not properly maintaining and cleaning the nails can create an environment that is conducive to fungal growth. Keeping nails excessively moist or regularly exposing them to hot and humid conditions, such as through excessive sweating or wearing tight-fitting shoes, can also promote fungal overgrowth.
Other risk factors include aging, as the nails become more brittle and dry with age, making them more vulnerable to fungal invasion. Trauma to the nails, such as from injury or repetitive pressure, can create small breaks or openings where fungi can enter. Furthermore, having a family history of nail infections may suggest a genetic predisposition to fungal susceptibility.
Overall, various risk factors such as weakened immune system, poor hygiene practices, age, trauma, and genetics contribute to why some individuals are more prone to nail infections caused by fungal pathogens. Understanding these factors can help in taking preventive measures and seeking appropriate treatment to minimize the risk and impact of nail infections.
Symptoms and signs of a fungal nail infection
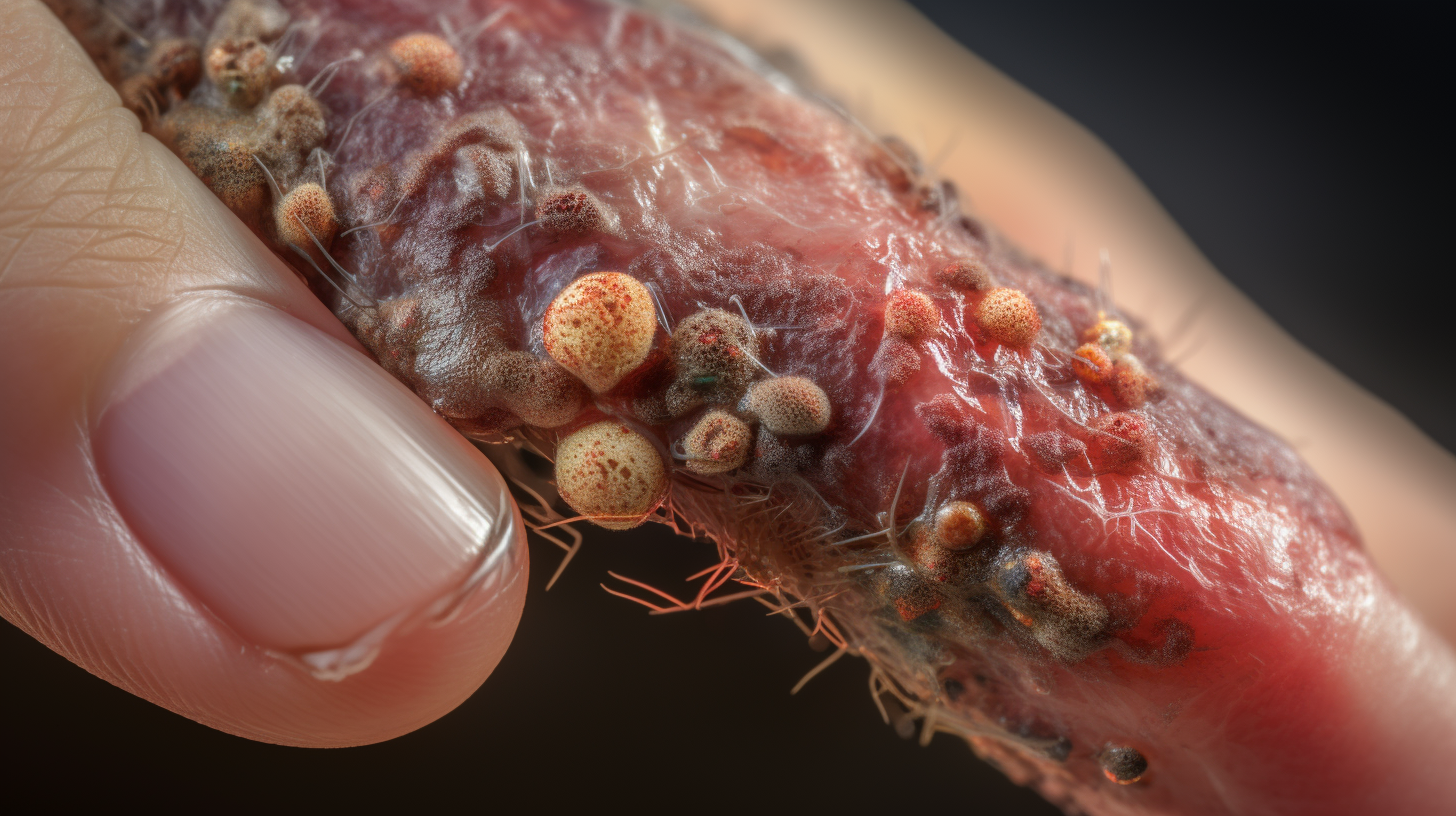
Fungal nail infections, also known as onychomycosis, occur when fungi invade the nail bed, causing an infection. Fungal pathogens are responsible for these nail infections and can affect both fingernails and toenails. Recognizing the symptoms and signs of a fungal nail infection is essential for early intervention and effective treatment.
The most common symptom of a fungal nail infection is a change in the appearance of the affected nail. Infected nails often become thickened, discolored (usually yellowish or brownish), and may develop a brittle or crumbly texture. Additionally, the infected nail may appear deformed, with irregular growth or shape. This change in the appearance of the nail is often accompanied by a foul odor.
Another common sign of a fungal nail infection is discomfort or pain in the affected area. As the infection progresses, the nail bed may become inflamed, causing tenderness and sensitivity. In some cases, the infection can lead to the separation of the nail from the nail bed, causing the affected nail to loosen or fall off entirely.
It’s important to note that fungal nail infections can be easily mistaken for other nail conditions, such as bacterial infections or psoriasis. Therefore, consulting a healthcare professional for an accurate diagnosis is recommended. Prompt treatment of fungal nail infections is crucial to prevent further spread of the infection and minimize potential complications.
Diagnosis: how healthcare professionals identify fungal pathogens in nail infections
In diagnosing nail infections caused by fungal pathogens, healthcare professionals employ a variety of methods to accurately identify the presence of these pathogens. One common diagnostic method is direct microscopy, where samples from the affected nail are examined under a microscope. This allows professionals to observe the morphology of the fungal pathogens, including the presence of hyphae or spores, which are characteristic traits of fungal infections.
Another approach is the culture of nail samples on specific growth media to promote the growth of the fungal pathogens. By isolating the pathogens and allowing them to multiply, healthcare professionals can identify the specific type of fungi causing the infection. This information is crucial in determining the appropriate treatment strategy, as different fungal pathogens may respond differently to antifungal medications.
Furthermore, healthcare professionals may also perform molecular tests such as polymerase chain reaction (PCR) to detect the genetic material of the fungal pathogens. PCR tests can provide rapid and highly accurate results, enabling prompt diagnosis and treatment initiation for patients with nail infections.
Ultimately, the accurate diagnosis of fungal pathogens in nail infections is essential for effective treatment planning. With a precise understanding of the causative fungi, healthcare professionals can tailor treatment regimens to target the specific pathogens and achieve better outcomes for patients.
Complications of untreated fungal nail infections
Fungal nail infections, also known as onychomycosis, can cause several complications if left untreated. Fungal pathogens, such as dermatophytes or yeasts, invade the nails and thrive in the warm and moist environment underneath them. If not addressed promptly, these infections can lead to various issues.
One common complication of untreated fungal nail infections is the thickening and distortion of the affected nail. As the infection progresses, the nail may become thick, brittle, and crumbly. The fungal invasion can cause the nail to warp and take on an abnormal shape, making it difficult to cut or maintain proper hygiene. In severe cases, the entire nail may detach from the nail bed or separate from the surrounding skin.
Another complication is the spread of the infection to other nails or nearby skin. Fungal pathogens can easily migrate from one nail to another, leading to multiple infected nails. Additionally, if the infection is not contained, it can extend to the surrounding skin, causing athlete’s foot or a rash known as dermatitis. These secondary infections can be challenging to treat and exacerbate the discomfort and cosmetic concerns associated with fungal nail infections.
Furthermore, untreated fungal nail infections can result in pain and discomfort. As the infection progresses, the affected nail and surrounding skin can become inflamed. This inflammation can lead to pain, tenderness, and even difficulty in walking or wearing shoes. In some cases, the discomfort can be so severe that it impacts an individual’s quality of life, limiting their ability to engage in daily activities.
Lastly, fungal nail infections can cause social and psychological implications. The appearance of discolored, thickened, and deformed nails can affect an individual’s self-esteem and confidence. People with untreated fungal nail infections may experience embarrassment or self-consciousness, leading to avoidance of social situations or wearing open-toed shoes. The psychological impact can be significant and have a negative impact on an individual’s overall well-being.
Given the potential complications associated with untreated fungal nail infections, it is crucial to seek medical attention and begin appropriate treatment as soon as symptoms appear. Early intervention can help prevent further complications and improve the chances of successful treatment and resolution of the infection.
Treatment options: medications, topical solutions, and home remedies
When it comes to treating fungal nail infections, there are several treatment options available, including medications, topical solutions, and home remedies. Medications are often the most effective treatment for these infections and can be prescribed by a healthcare professional. Oral antifungal medications, such as terbinafine or itraconazole, are commonly prescribed to treat nail infections. These medications work by targeting the fungus causing the infection and help in promoting the growth of a healthy nail. It is important to follow the prescribed dosage and complete the full course of treatment to ensure the complete eradication of the infection.
Topical solutions are another option for treating fungal nail infections. These solutions usually contain antifungal agents like amorolfine or ciclopirox, which need to be applied directly to the affected nail. These solutions can penetrate the nail and reach the underlying infection, effectively killing the fungus. However, topical treatments tend to be less effective than oral medications, and treatment may take longer to see results.
In addition to medications and topical solutions, there are also various home remedies that can help alleviate the symptoms and promote healing. Soaking the affected nails in a mixture of warm water and vinegar or applying tea tree oil to the nails are popular home remedies believed to have antifungal properties. However, it is important to note that home remedies may not be as effective as prescription medications or topical solutions and should be used in conjunction with professional treatment.
It is crucial to consult a healthcare professional for an accurate diagnosis and proper treatment of fungal nail infections. They can recommend the most appropriate treatment option based on the severity of the infection and individual circumstances. It is also essential to maintain good foot hygiene, including keeping nails trimmed and dry, to prevent the recurrence of fungal nail infections.
Preventing fungal nail infections: essential tips for maintaining healthy nails
Fungal nail infections, also known as onychomycosis, can be a bothersome and persistent condition. Understanding the causes of these infections is crucial in preventing their occurrence. Fungal pathogens, such as dermatophytes and yeasts, are responsible for nail infections. These microorganisms thrive in warm, moist environments, making the nails an ideal breeding ground.
To maintain healthy nails and prevent fungal infections, there are several essential tips to follow. Firstly, practicing good hygiene is paramount. Regularly washing and drying the feet thoroughly, especially between the toes, can help eliminate excess moisture that can promote fungal growth. It is also advisable to wear clean, breathable footwear and change socks daily to prevent moisture buildup.
In addition to hygiene, proper nail care is vital for preventing fungal infections. Keeping nails trimmed, short, and clean can minimize the chances of microorganisms entering and thriving underneath the nail plate. It is equally important to avoid sharing personal items like nail clippers or files, as this can lead to cross-contamination.
Overall, taking preventative measures to maintain healthy nails is key to avoiding fungal nail infections. By following these essential tips, individuals can reduce the risk of fungal pathogens causing nail infections and enjoy healthy, strong nails. If an infection does occur, seeking prompt medical attention from a healthcare professional is crucial for effective treatment.
Seeking professional help: when to visit a healthcare professional for nail infections
Fungal pathogens can cause nail infections, also known as onychomycosis, which can be bothersome and stubborn to treat. While some cases of mild nail infections can be treated with over-the-counter antifungal creams and ointments, seeking professional help is recommended in certain situations.
One indication for visiting a healthcare professional is if the infection spreads to other nails or the surrounding skin. Fungal nail infections can easily spread and cause further damage if left untreated. A healthcare professional can provide a proper diagnosis and recommend effective treatment options to prevent the infection from worsening and spreading.
Another instance where professional help is necessary is when there are underlying health conditions present, such as diabetes, weakened immune system, or circulatory disorders. These conditions can compromise the body’s ability to fight off infections, making it even harder to treat nail infections successfully. Seeking the expertise of a healthcare professional can ensure that the treatment plan is tailored to the individual’s specific health needs.
Furthermore, if over-the-counter treatments have been unsuccessful in treating the nail infection within a reasonable period, it is advisable to consult a healthcare professional. They can assess the severity of the infection and prescribe stronger antifungal medications or other therapies that may be more effective.
In conclusion, while some nail infections can be managed with over-the-counter treatments, it is essential to seek professional help in certain circumstances. It is particularly crucial when the infection spreads, underlying health conditions are present, or over-the-counter treatments are ineffective. By visiting a healthcare professional, individuals can receive proper diagnosis and tailored treatment plans to effectively manage and treat their nail infections.
Lifestyle and hygiene practices to minimize the risk of fungal nail infections
Fungal nail infections can be prevented or minimized by adopting certain lifestyle and hygiene practices. Firstly, it is important to maintain good foot hygiene by regularly washing and drying your feet thoroughly. Fungal organisms thrive in warm and moist environments, so keeping your feet clean and dry can help minimize their growth. It is particularly important to dry the feet, including between the toes, as these areas are prone to trapping moisture.
Wearing well-fitting shoes made of breathable materials, such as leather or canvas, can also help reduce the risk of fungal nail infections. This allows air circulation around the feet, preventing excessive sweating and moisture build-up. Additionally, avoiding tight and closed-toe footwear for long durations, especially in hot and humid environments, can help create an unfavorable environment for fungal growth.
Practicing good nail care is another crucial aspect of preventing fungal nail infections. Keep your nails neatly trimmed, cutting them straight across and avoiding excessively short cuts or rounded edges. It is important to use clean and sterilized nail clippers or scissors, as shared tools can contribute to the spread of fungal infections. Moreover, avoiding nail trauma or injury is essential, as it can create openings in the nail bed that allow fungal pathogens to enter and cause infections.
Furthermore, it is advisable to change socks and shoes regularly, particularly after participating in activities that cause excessive sweating. Moisture-wicking socks made of natural fibers like cotton or wool can help absorb sweat and keep the feet dry. It is also recommended to avoid sharing personal items such as socks, shoes, towels, or nail care tools, as these can facilitate the transmission of fungal pathogens.
By adopting these lifestyle and hygiene practices, you can significantly minimize the risk of fungal nail infections. However, if you suspect you have a fungal nail infection or notice any changes in your nails, it is important to consult a healthcare professional for proper diagnosis and treatment.
Conclusion: understanding the causes and prevention of fungal nail infections
In conclusion, understanding the causes and prevention of fungal nail infections is crucial for effectively managing and treating this common condition. Fungal pathogens primarily cause nail infections by penetrating the nail plate and colonizing the underlying tissues. Factors such as a weakened immune system, moist and warm environments, and pre-existing nail abnormalities can increase the risk of developing nail infections.
To prevent fungal nail infections, it is important to maintain good hygiene practices. This includes keeping the nails clean and dry, avoiding prolonged exposure to moist environments (such as public swimming pools or communal showers), and wearing breathable footwear. Regularly trimming the nails and avoiding tight-fitting shoes can also help reduce the chances of infection.
Additionally, individuals should take care to protect their nails from trauma and injuries, as these can create entry points for fungal pathogens. Using antifungal powders or creams on the nails and feet can provide an added layer of protection against fungal infections.
Overall, by understanding the causes and implementing preventive measures, individuals can greatly reduce the risk of developing fungal nail infections. Prompt diagnosis and treatment are also essential in managing this condition effectively.
Leave a Reply